While not as famous and well understood as its close neighbor, the thyroid gland, the thymus gland has a short lifespan but a huge impact on the human body. Unlike other glands that work to produce the hormones the body needs in order to perform specific functions for the duration of a person’s life, the thymus gland is only active until the body reaches puberty, at which point it begins to shrink and transform into fat.
The thymus gland may only be active in the body for a little over a decade or so depending on the person, but the work it does is literally responsible for human survival, from birth until well into adulthood and old age.
The Brief, Wondrous Life of the Thymus Gland
Back in 1982, almost a full decade before the inception of the Human Genome Project and well before the concept of regenerative medicine hit the mainstream, The New York Times published an article pondering the thymus gland’s role in the aging process. Given the research as well as medical and commercial applications that would follow in the decades after the article was first published, some of the author’s questions and ideas now seem downright prophetic:
“Research on the immune defenses’ decline with age has focused new attention on a pinkish-gray two-lobed organ called the thymus gland. Mysteriously, the thymus begins its own decline when many organs are still growing. Does that early decline lead the way in an inexorable chain of events that weakens the defenses of the aging human body? Is it a key event in aging itself? And, if so, might replacement of some of the gland’s products slow the process?
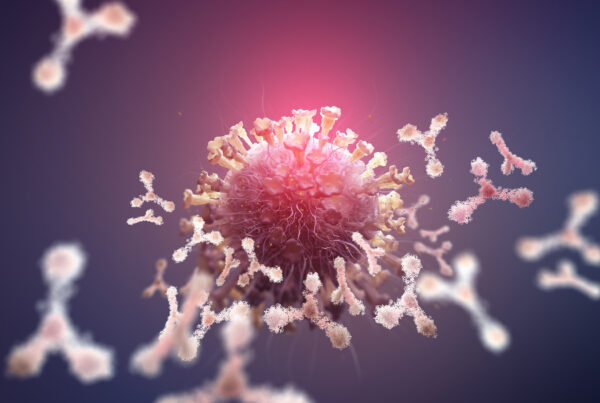
The thymus is a target of research on these issues because of its important and complex functions in the immune system. It processes a broad category of immunologically active white blood cells, called Tcells or T-lymphocytes because they pass through the thymus and are modified there before coming to maturity. Thereafter many populations of T cells serve in a complex array of roles – killing invaders, enhancing some immune functions while suppressing others, helping antibody-producing cells recognize antibody targets. The thymus also makes at least four different hormones that have been discovered and purified in recent years.”
As it turned out, replacing some of the thymus gland’s products, like the protein thymosin beta 4, and other cellular processes to help fight disease and improve health, especially as we age, is at the core of peptide therapy.
 What is Thymosin Beta 4?
What is Thymosin Beta 4?
One of the thymus gland’s products is the polypeptide hormone thymosin, which is primarily responsible for creating T cells, which are a staple of the immune system and the body’s ability to fight off infection and disease. Thymosin constitutes a family of hormones, so there are many subtypes of the protein.
Thymosin beta 4 is known as the most “abundant” member of the cell type due to the fact that the protein is expressed in multiple cell types in mammals, and plays a role in many key biological processes. Some of the protein’s many roles include:
- Organization of the cytoskeleton
- Cell migration
- Formation of blood vessels
- Cell survival
- Stem cell differentiation
- Gene expression
- Anti-inflammatory agent
Thymosin beta 4 also plays a role in clot formation, and it is currently used along with other clinical therapies to treat certain types of myocardial infarction (heart attack). Thymosin beta 4’s regenerative properties also make it a natural agent in the process of wound healing.
According to a paper published in the Vitamins and Hormones journal summarizing the findings of recent experiments into the regenerative properties and potential clinical applications for Thymosin beta 4:
“Thymosin beta 4 (Tβ4) is a small, abundant, naturally occurring regenerative protein that is found in body fluids and inside cells. It was found to have angiogenic and anti-inflammatory activity and to be high in platelets that aggregate at the wound site. Thus we used Tβ4 initially in dermal healing.
It has since been shown to have many activities important in tissue protection, repair, and regeneration. Tβ4 increases the rate of dermal healing in various preclinical animal models, including diabetic and aged animals, and is active for burns as well. Tβ4 also accelerated the rate of repair in phase 2 trials with patients having pressure ulcers, stasis ulcers, and epidermolysis bullosa wounds. It is safe and well tolerated and will likely have additional uses in the skin and in injured organs for tissue repair and regeneration.”
Due to its anti-inflammatory and regenerative properties, thymosin beta 4 researchers have spent the last few decades studying how it may be used in a therapeutic capacity to potentially help treat many of the injuries and illnesses that stem from common health problems like inflammation and weakened immune function.
What is Thymosin Alpha 1?
While this post will focus on Thymosin Beta 4, it’s important to bring up another peptide that is often confused with TB4, Thymosin Alpha 1. TA1 has immune-boosting features – to the extent that a patented version exists called Zadaxin. In this form, it is used in the treatment of Chronic Hepatitis A and C.
Inflammation: What Is It and Why Is It So Bad for Your Health?
By now most people know that inflammation is dangerous and can increase the risk of a number of serious health problems and diseases, from heart problems to cancer. But what exactly is it, what causes it, and how does it lead to disease?
Inflammation is actually a normal immune response to illness, trauma, or infection. Whenever you cut your hand, twist your ankle, or pick up the flu virus or bacterial infection, the immune system is triggered and releases white blood cells to help you fight off the infection or injury. This is the body’s normal inflammatory response to foreign intruders that put your health at risk.
However just like the fight or flight response, inflammation is meant to be temporary until the wound has healed or the infection has cleared up. When the inflammatory response goes into overdrive and becomes chronic (long term), it actually can have the opposite effect and can actually put your health at risk in a number of ways.
Common Factors That Can Lead to Chronic Inflammation in the Body
When your body is constantly in fight mode, it can overwhelm your immune system to the point where it actually triggers diseases and health problems. According to the Cleveland Clinic, chronic inflammation can increase the risk of a number of serious health problems including:
- Arterial plaque buildup (increasing your risk of heart attack and stroke)
- Alzheimer’s disease (plaque buildup in the brain)
- Organ damage
- Cancer
In addition to plaque buildup, chronic inflammation also causes cellular damage and can set off a chain reaction that may play a role in the development of several forms of cancer. According to the Cancer Treatment Centers of America:
“Chronic inflammation’s role in cancer development isn’t a small one. As many as one in five cancers are believed to be caused or influenced by inflammation. One reason is that chronic inflammation may damage DNA, says Cynthia Lynch, MD, Medical Director of the CTCA® Breast Cancer Center, Phoenix and Medical Oncologist at our Phoenix hospital. Other times, the inflammatory process produces molecules called cytokines, which stimulate the growth of blood vessels that bring oxygen and nutrients to the tumor. The process also may generate molecules called free radicals that further damage the DNA. These inflammation side effects may help sustain and fuel cancer growth.
The reason inflammation becomes chronic isn’t always apparent. It may be caused by infections that don’t go away, abnormal immune reactions to normal tissues, or certain conditions like obesity. Over time, chronic inflammation may damage DNA, leading to conditions like heart disease, type 2 diabetes, stroke and cancer. “Anything that causes inflammation will cause the DNA of a cell to replicate faster,” says Brad Mons, DO, Head and Neck Surgeon at our hospital in Tulsa. “The more your cells replicate, the higher chance you have of cancers developing.””
In addition to heart disease and cancer, chronic inflammation can increase the risk of other health problems.
 What You Can Do to Control Your Risk of Chronic Inflammation
What You Can Do to Control Your Risk of Chronic Inflammation
The good news is that there are several proactive steps you can take to lower your risk of developing chronic inflammation — and the potentially serious and life-threatening health risks that come along with it.
The lifestyle factors that play a role in chronic inflammation are the usual suspects:
- Obesity
- Smoking
- Excessive alcohol consumption
- Long term/chronic stress
Eating a healthy, anti-inflammatory diet like the Mediterranean diet, not smoking, drinking alcohol in moderation, exercising, maintaining a healthy weight, and managing stress can help to keep chronic inflammation at bay.
Additional Causes of Inflammation
Underlying health conditions like certain types of infections and environmental exposure to toxins and pollutants are additional factors that can lead to chronic inflammation in the body.
Tb 500 Peptide Therapy
Tb 500 is a synthetic derivative of thymosin beta 4 used to help enhance the healing response, specifically in soft tissue injuries like tendon and ligament tears. It is contained within TB4, but cannot be acquired directly.
It also acts as an anti-inflammatory agent like thymosin beta 4. Peptides consist of a string of different amino acids of varying lengths. Peptide therapy allows scientists to replicate and rearrange peptides that don’t form on their own in the body. In the case of thymosin beta 4, which consists of 43 amino acid blocks, tb 500 is made from a smaller portion of the naturally occurring peptide.
According to a paper published by the US National Library of Medicine, National Institutes of Health on the role of thymosin peptide on tissue repair and regeneration:
“Studies in various animal models of disease and repair with thymosin beta(4) (Tbeta(4)), the major actin-sequestering molecule in mammalian cells, have provided the scientific foundation for the ongoing dermal, corneal, and cardiac wound repair multicenter clinical trials. Tbeta(4) has of multiple biological activities, which include down-regulation of inflammatory chemokines and cytokines, and promotion of cell migration, blood vessel formation, cell survival, and stem cell maturation. All of these activities contribute to the multiple wound healing properties that have been observed in animal studies.”
Tb 500 is typically administered through a subcutaneous injection, but it can also be injected into muscle tissue for an average of two to three injections per week. Due to its potential to help with healing and anti-inflammatory properties, tb 500 may be a good option for highly active individuals looking to supplement recovery from sports or overuse injuries, for example.
Since Tb500 cannot be acquired legally, thymosin beta 4 is typically used in its stead.
In general, the reported side effects for peptide therapy treatments like tb 500 are relatively low. As with any injectable, some people may experience discomfort or mild swelling at the injection site. Other potential side effects of tb 500 may include nausea, vomiting, and lightheadedness.
As with any treatment, the results and potential side effects of peptide therapy will vary from person to person. Peptide therapy is not intended as a replacement or alternative to medical treatment or a healthy diet and active lifestyle, which is the cornerstone of lasting health, wellbeing, and longevity. For high functioning and athletic individuals, peptide therapy may provide an added boost to traditional therapies and treatment programs.
Peptide therapy is an exciting field with numerous opportunities for medical breakthroughs based on the natural pathways and processes that the human body uses to recover from wounds and injuries and to fight off infection and disease. From lifestyle factors that increase the risk of disease, to the aging process itself, a healthy immune system is the first and best line of defense. Peptide therapy aims to help keep that process as efficient as possible.
If you’re interested in learning more about the effects and benefits of thymosin beta 4 (TB4) and peptide therapy, contact us today for more information.


 What is Thymosin Beta 4?
What is Thymosin Beta 4? What You Can Do to Control Your Risk of Chronic Inflammation
What You Can Do to Control Your Risk of Chronic Inflammation